Pes Planus Causes, Signs Or Symptoms And Therapies
Overview

A quarter of Americans have flat feet. While most people with flat feet don't have serious problems as a result, for some, flat feet can cause disabling foot pain as well as knee pain, shin splints, Achilles tendinitis, and plantar fasciitis. A person with foot or leg pain should pay particular attention to whether one foot is flatter than the other.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Feet tire easily and become painful and achy, especially around the arch, ankle and heel. Swelling on the inside bottom of your feet. Back and leg pain. Difficulty standing on toes.
Diagnosis
There are a few simple ways to assess your foot type, and most include making an imprint of your footprint. The classic way is to stand on a hard floor surface with wet feet to make a wet foot print. Look at the narrowest part of your footprint, which should be between your heel and ball of your foot. If the print of your foot in this part is less than 10% of the width of the widest part then you are likely to have high arches. more than 10% but less than 25% then your foot profile is probably normal, more than 25% or even the widest part, then you have flat feet.
pes valgus
Non Surgical Treatment
The type of treatment will depend on the stage of PTTD present. There are four stages of posterior tibial tendon dysfunction. Stage I. The posterior tibial tendon is inflamed but has normal strength. There is little to no change in the arch of the foot. The patient can still perform a single-limb heel rise and has a flexible hindfoot. Orthotic treatment options include modified off the shelf inserts and custom molded orthotics. Stage 2. The tendon is partially torn or shows degenerative changes and as a result loses strength.There is considerable flattening of the arch without arthritic changes in the foot. The patient cannot perform single-limb heel rise. Pain is now present on the lateral aspect of the ankle. Orthotic treatment is similar as that in stage I, with the addition of more rigid arch supports and wedging. Stage 3. Results when the posterior tibial tendon is torn and not functioning. As a result the arch is completely collapsed with arthritic changes in the foot. A solid ankle AFO is suggested in conjunction with a modified orthopedic shoe. Stage 4. Is identical to stage three except that the ankle joint also becomes arthritic. A rigid AFO and modified orthopedic shoe is required.
Surgical Treatment

Surgical procedures for flat feet vary depending on the root cause of the condition. Surgical correction to control pronation may include bone implants or Achilles tendon lengthening. Tendon transfer, which is a procedure to re-attach a tendon to another area of bone, may also be used to reduce pronation and improve foot function.
Prevention
It?s time to take a long hard look at what?s in your closet. Now is the time to toss out shoes that are well worn. You also need to say good-bye to thin-soled shoes that offer zero arch support. If you?re overweight, fallen arches may be a sign the universe is trying to tell you something. You need to lose weight, and odds are, fallen arches are but one of many physical discomforts you are experiencing.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.

A quarter of Americans have flat feet. While most people with flat feet don't have serious problems as a result, for some, flat feet can cause disabling foot pain as well as knee pain, shin splints, Achilles tendinitis, and plantar fasciitis. A person with foot or leg pain should pay particular attention to whether one foot is flatter than the other.
Causes
Fallen arches have many causes. If you have fallen arches, or flat feet, the normal arch in the middle of your foot is not curved properly. You can have this condition called ples planus in medical terms and never have any symptoms. However, fallen arches can lead to foot pain, fatigue or more serious conditions. If fallen arches alter the way you walk, you may eventually develop knee, hip and low back pain. Your foot may lose normal range of motion making it hard to rise up onto your toes. In some cases, your feet can become swollen. If you have this condition, talk to your doctor about an appropriate treatment plan.
Symptoms
Feet tire easily and become painful and achy, especially around the arch, ankle and heel. Swelling on the inside bottom of your feet. Back and leg pain. Difficulty standing on toes.
Diagnosis
There are a few simple ways to assess your foot type, and most include making an imprint of your footprint. The classic way is to stand on a hard floor surface with wet feet to make a wet foot print. Look at the narrowest part of your footprint, which should be between your heel and ball of your foot. If the print of your foot in this part is less than 10% of the width of the widest part then you are likely to have high arches. more than 10% but less than 25% then your foot profile is probably normal, more than 25% or even the widest part, then you have flat feet.
pes valgus
Non Surgical Treatment
The type of treatment will depend on the stage of PTTD present. There are four stages of posterior tibial tendon dysfunction. Stage I. The posterior tibial tendon is inflamed but has normal strength. There is little to no change in the arch of the foot. The patient can still perform a single-limb heel rise and has a flexible hindfoot. Orthotic treatment options include modified off the shelf inserts and custom molded orthotics. Stage 2. The tendon is partially torn or shows degenerative changes and as a result loses strength.There is considerable flattening of the arch without arthritic changes in the foot. The patient cannot perform single-limb heel rise. Pain is now present on the lateral aspect of the ankle. Orthotic treatment is similar as that in stage I, with the addition of more rigid arch supports and wedging. Stage 3. Results when the posterior tibial tendon is torn and not functioning. As a result the arch is completely collapsed with arthritic changes in the foot. A solid ankle AFO is suggested in conjunction with a modified orthopedic shoe. Stage 4. Is identical to stage three except that the ankle joint also becomes arthritic. A rigid AFO and modified orthopedic shoe is required.
Surgical Treatment

Surgical procedures for flat feet vary depending on the root cause of the condition. Surgical correction to control pronation may include bone implants or Achilles tendon lengthening. Tendon transfer, which is a procedure to re-attach a tendon to another area of bone, may also be used to reduce pronation and improve foot function.
Prevention
It?s time to take a long hard look at what?s in your closet. Now is the time to toss out shoes that are well worn. You also need to say good-bye to thin-soled shoes that offer zero arch support. If you?re overweight, fallen arches may be a sign the universe is trying to tell you something. You need to lose weight, and odds are, fallen arches are but one of many physical discomforts you are experiencing.
After Care
Time off work depends on the type of work as well as the surgical procedures performed. . A patient will be required to be non-weight bearing in a cast or splint and use crutches for four to twelve weeks. Usually a patient can return to work in one to two weeks if they are able to work while seated. If a person's job requires standing and walking, return to work may take several weeks. Complete recovery may take six months to a full year. Complications can occur as with all surgeries, but are minimized by strictly following your surgeon's post-operative instructions. The main complications include infection, bone that is slow to heal or does not heal, progression or reoccurrence of deformity, a stiff foot, and the need for further surgery. Many of the above complications can be avoided by only putting weight on the operative foot when allowed by your surgeon.
All You Should Know About
Overview

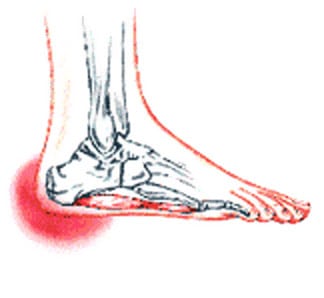
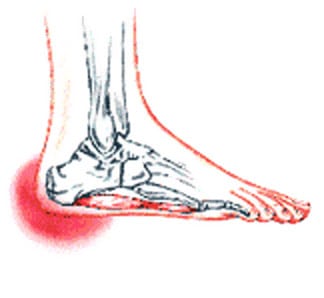
The most common cause of heel pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
The most common cause of heel pain is plantar fasciitis. Plantar fasciitis is a stretching of the plantar fascia, a ligament that runs from the ball of foot through the arch and is attached to the heel. It is that attachment which becomes aggravated and typically causes pain after being on your feet for lengths of time. Abnormal motion of the foot (pronation) is one cause of plantar fasciitis. Heel spurs, which are abnormal bone growths coming off the heel, can also cause heel pain. Other causes include repetitive stress or shock to the heel, standing for prolonged periods or osteoarthritis.
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Home care, in cases that are not severe, home care is probably enough to get rid of heel pain. Rest, avoid running or standing for long periods, or walking on hard surfaces. Avoid activities that may stress the heels. Ice, place an ice-pack on the affected area for about 15 minutes. Do not place bare ice directly onto skin. Footwear. proper-fitting shoes that provide good support are crucial. Athletes should be particularly fussy about the shoes they use when practicing or competing - sports shoes need to be replaced at specific intervals (ask your trainer). Foot supports, wedges and heel cups can help relieve symptoms.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
replacement ankle straps for heels
Prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.

The most common cause of heel pain is plantar fasciitis which is commonly referred to as a heel spur. Plantar fascia is a broad band of fibrous tissue which runs along the bottom surface of the foot, from the heel to the toes. Plantar fasciitis is a condition in which the plantar fascia is inflamed. This condition can be very painful and cause a considerable amount of suffering.
Causes
The most common cause of heel pain is plantar fasciitis. Plantar fasciitis is a stretching of the plantar fascia, a ligament that runs from the ball of foot through the arch and is attached to the heel. It is that attachment which becomes aggravated and typically causes pain after being on your feet for lengths of time. Abnormal motion of the foot (pronation) is one cause of plantar fasciitis. Heel spurs, which are abnormal bone growths coming off the heel, can also cause heel pain. Other causes include repetitive stress or shock to the heel, standing for prolonged periods or osteoarthritis.
Symptoms
Depending on the specific form of heel pain, symptoms may vary. Pain stemming from plantar fasciitis or heel spurs is particularly acute following periods of rest, whether it is after getting out of bed in the morning, or getting up after a long period of sitting. In many cases, pain subsides during activity as injured tissue adjusts to damage, but can return again with prolonged activity or when excessive pressure is applied to the affected area. Extended periods of activity and/or strain of the foot can increase pain and inflammation in the foot. In addition to pain, heel conditions can also generate swelling, bruising, and redness. The foot may also be hot to the touch, experience tingling, or numbness depending on the condition.
Diagnosis
A biomechanical exam by your podiatrist will help reveal these abnormalities and in turn resolve the cause of plantar fasciitis. By addressing this cause, the patient can be offered a podiatric long-term solution to his problem.
Non Surgical Treatment
Home care, in cases that are not severe, home care is probably enough to get rid of heel pain. Rest, avoid running or standing for long periods, or walking on hard surfaces. Avoid activities that may stress the heels. Ice, place an ice-pack on the affected area for about 15 minutes. Do not place bare ice directly onto skin. Footwear. proper-fitting shoes that provide good support are crucial. Athletes should be particularly fussy about the shoes they use when practicing or competing - sports shoes need to be replaced at specific intervals (ask your trainer). Foot supports, wedges and heel cups can help relieve symptoms.
Surgical Treatment
It is rare to need an operation for heel pain. It would only be offered if all simpler treatments have failed and, in particular, you are a reasonable weight for your height and the stresses on your heel cannot be improved by modifying your activities or footwear. The aim of an operation is to release part of the plantar fascia from the heel bone and reduce the tension in it. Many surgeons would also explore and free the small nerves on the inner side of your heel as these are sometimes trapped by bands of tight tissue. This sort of surgery can be done through a cut about 3cm long on the inner side of your heel. Recently there has been a lot of interest in doing the operation by keyhole surgery, but this has not yet been proven to be effective and safe. Most people who have an operation are better afterwards, but it can take months to get the benefit of the operation and the wound can take a while to heal fully. Tingling or numbness on the side of the heel may occur after operation.
replacement ankle straps for heels
Prevention
A variety of steps can be taken to avoid heel pain and accompanying afflictions. Wear shoes that fit well-front, back, and sides-and have shock-absorbent soles, rigid shanks, and supportive heel counters. Wear the proper shoes for each activity. Do not wear shoes with excessive wear on heels or soles. Prepare properly before exercising. Warm up and do stretching exercises before and after running. Pace yourself when you participate in athletic activities. Don't underestimate your body's need for rest and good nutrition. If obese, lose weight.
Sole Lifts For Leg Length Discrepancy
Overview
Bone growth restriction (epiphysiodesis) The objective of this surgical procedure is to slow down growth in the longer leg. During surgery, doctors alter the growth plate of the bone in the longer leg by inserting a small plate or staples. This slows down growth, allowing the shorter leg to catch up over time. Your child may spend a night in the hospital after this procedure or go home the same day. Doctors may place a knee brace on the leg for a few days. It typically takes 2 to 3 months for the leg to heal completely. An alternative approach involves lengthening the shorter bone. We are more likely to recommend this approach if your child is on the short side of the height spectrum.
Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
A properly made foot orthotic can go a long way in substituting additional millimeters or centimeter on the deficient side. Additional full length inserts are added to the shorter side bringing the runner closer to symmetrical. Heel lifts do not work in runners because when you run you may land on your heel but the rest of the time you are on your forefoot then your toes pushing off. The right custom-made, biomechanical orthotic can address the underlying cause of your pain. Abnormal joint position, overpronation or foot rigidity can be addressed and the biomechanics normalized. San Diego Running Institute orthotics are custom molded to your foot and are designed with your specific body weight, leg length discrepancy, and activity in mind. The restoration of correct mechanical function takes the abnormal stress from the uneven side and allows the body to heal naturally.

deelsonheels
Surgical Treatment
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.
Bone growth restriction (epiphysiodesis) The objective of this surgical procedure is to slow down growth in the longer leg. During surgery, doctors alter the growth plate of the bone in the longer leg by inserting a small plate or staples. This slows down growth, allowing the shorter leg to catch up over time. Your child may spend a night in the hospital after this procedure or go home the same day. Doctors may place a knee brace on the leg for a few days. It typically takes 2 to 3 months for the leg to heal completely. An alternative approach involves lengthening the shorter bone. We are more likely to recommend this approach if your child is on the short side of the height spectrum.

Causes
The causes of LLD are many, including a previous injury, bone infection, bone diseases (dysplasias), inflammation (arthritis) and neurologic conditions. Previously broken bones may cause LLD by healing in a shortened position, especially if the bone was broken in many pieces (comminuted) or if skin and muscle tissue around the bone were severely injured and exposed (open fracture). Broken bones in children sometimes grow faster for several years after healing, causing the injured bone to become longer. Also, a break in a child?s bone through a growth center (located near the ends of the bone) may cause slower growth, resulting in a shorter extremity. Bone infections that occur in children while they are growing may cause a significant LLD, especially during infancy. Bone diseases may cause LLD, as well; examples are neurofibromatosis, multiple hereditary exostoses and Ollier disease. Inflammation of joints during growth may cause unequal extremity length. One example is juvenile rheumatoid arthritis. Osteoarthritis, the joint degeneration that occurs in adults, very rarely causes a significant LLD.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
On standing examination one iliac crest may be higher/lower than the other. However a physiotherapist, osteopath or chiropractor will examine the LLD in prone or supine position and measure it, confirming the diagnosis of structural (or functional) LLD. The LLD should be measured using bony fixed points. X-Ray should be taken in a standing position. The osteopath, physiotherapist or chiropractor will look at femoral head & acetabulum, knee joints, ankle joints.
Non Surgical Treatment
A properly made foot orthotic can go a long way in substituting additional millimeters or centimeter on the deficient side. Additional full length inserts are added to the shorter side bringing the runner closer to symmetrical. Heel lifts do not work in runners because when you run you may land on your heel but the rest of the time you are on your forefoot then your toes pushing off. The right custom-made, biomechanical orthotic can address the underlying cause of your pain. Abnormal joint position, overpronation or foot rigidity can be addressed and the biomechanics normalized. San Diego Running Institute orthotics are custom molded to your foot and are designed with your specific body weight, leg length discrepancy, and activity in mind. The restoration of correct mechanical function takes the abnormal stress from the uneven side and allows the body to heal naturally.

deelsonheels
Surgical Treatment
Surgeries for LLD are designed to do one of three general things ? shorten the long leg, stop or slow the growth of the longer or more rapidly growing leg, or lengthen the short leg. Stopping the growth of the longer leg is the most commonly utilized of the three approaches and involves an operation known as an epiphysiodesis , in which the growth plate of either the lower femur or upper tibia is visualized in the operating room using fluoroscopy (a type of real-time radiographic imaging) and ablated , which involves drilling into the region several times, such that the tissue is no longer capable of bone growth. Because the epiphyseal growth capabilities cannot be restored following the surgery, proper timing is crucial. Usually the operation is planned for the last 2 to 3 years of growth and has excellent results, with children leaving the hospital within a few days with good mobility. However, it is only appropriate for LLD of under 5cm.
How To Estimate Anatomical Leg Length Discrepancy
Overview
There are generally two kinds of leg length discrepancies. Structural discrepancy occurs when either the thigh (femur) or shin (tibia) bone in one leg is actually shorter than the corresponding bone in the other leg. Functional discrepancy occurs when the leg lengths are equal, but symmetry is altered somewhere above the leg, which in turn disrupts the symmetry of the legs. For example, developmental dislocation of the hip (DDH) can cause a functional discrepancy. In DDH, the top of the leg bone (femur) that is not properly positioned in the hip socket may hang lower than the femur on the other side, giving the appearance and symptoms of a leg length discrepancy.
Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
In order to measure for correction, use a series of blocks or sheets of firm material (cork or neoprene) of varying thickness, e.g., 1/8", 1/4", and 1/2". Place them under the short limb, either under the heel or the entire foot, depending on the pathology, until the patient feels most balanced. Usually you will not be able to correct for the full amount of the imbalance at the outset. The longer a patient has had the LLD, the less likely he or she will be able to tolerate a full correction immediately. This is a process of incremental improvements. 2 inch External Platform Lift Bear in mind that the initial lift may need to be augmented as the patient's musculoskeletal system begins to adjust. It is often recommended that the initial buildup should be 50 percent of the total. After a suitable break-in period, one month say, another 25 percent can be added. If warranted, the final 25 percent can be added a month later. Once you determine how much lift the patient can handle, you then need to decide how to best apply it. There are certain advantages and disadvantages to using either internal or external heel lifts.

bestshoelifts
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
There are generally two kinds of leg length discrepancies. Structural discrepancy occurs when either the thigh (femur) or shin (tibia) bone in one leg is actually shorter than the corresponding bone in the other leg. Functional discrepancy occurs when the leg lengths are equal, but symmetry is altered somewhere above the leg, which in turn disrupts the symmetry of the legs. For example, developmental dislocation of the hip (DDH) can cause a functional discrepancy. In DDH, the top of the leg bone (femur) that is not properly positioned in the hip socket may hang lower than the femur on the other side, giving the appearance and symptoms of a leg length discrepancy.

Causes
A number of causes may lead to leg length discrepancy in children. Differences in leg length frequently follow fractures in the lower extremities in children due to over or under stimulation of the growth plates in the broken leg. Leg length discrepancy may also be caused by a congenital abnormality associated with a condition called hemihypertrophy. Or it may result from neuromuscular diseases such as polio and cerebral palsy. Many times, no cause can be identified. A small leg length discrepancy of a quarter of an inch or less is quite common in the general population and of no clinical significance. Larger leg length discrepancies become more significant. The long-term consequences of a short leg may include knee pain, back pain, and abnormal gait or limp.
Symptoms
Many people walk around with LLD?s of up to 2 cm. and not even know it. However, discrepancies above 2 cm. becomes more noticeable, and a slight limp is present. But even up to 3 cm. a small lift compensates very well, and many patients are quite happy with this arrangement. Beyond 3 cm. however, the limp is quite pronounced, and medical care is often sought at that point. Walking with a short leg gait is not only unsightly, but increases energy expenditure during ambulation. It could also put more stress on the long leg, and causes functional scoliosis. Where the discrepancy is more severe, walking becomes grotesque or virtually impossible.
Diagnosis
A systematic and well organized approach should be used in the diagnosis of LLD to ensure all relevant factors are considered and no clues are overlooked which could explain the difference. To determine the asymmetry a patient should be evaluated whilst standing and walking. During the process special care should be used to note the extent of pelvic shift from side to side and deviation along the plane of the front or leading leg as well as the traverse deviation of the back leg and abnormal curvature of the spine. Dynamic gait analysis should be conducted during waling where observation of movement on the sagittal, frontal and transverse planes should be noted. Also observe head, neck and shoulder movements for any tilting.
Non Surgical Treatment
In order to measure for correction, use a series of blocks or sheets of firm material (cork or neoprene) of varying thickness, e.g., 1/8", 1/4", and 1/2". Place them under the short limb, either under the heel or the entire foot, depending on the pathology, until the patient feels most balanced. Usually you will not be able to correct for the full amount of the imbalance at the outset. The longer a patient has had the LLD, the less likely he or she will be able to tolerate a full correction immediately. This is a process of incremental improvements. 2 inch External Platform Lift Bear in mind that the initial lift may need to be augmented as the patient's musculoskeletal system begins to adjust. It is often recommended that the initial buildup should be 50 percent of the total. After a suitable break-in period, one month say, another 25 percent can be added. If warranted, the final 25 percent can be added a month later. Once you determine how much lift the patient can handle, you then need to decide how to best apply it. There are certain advantages and disadvantages to using either internal or external heel lifts.

bestshoelifts
Surgical Treatment
Surgical treatments vary in complexity. Sometimes the goal of surgery is to stop the growth of the longer limb. Other times, surgeons work to lengthen the shorter limb. Orthopedic surgeons may treat children who have limb-length conditions with one or a combination of these surgical techniques. Bone resection. An operation to remove a section of bone, evening out the limbs in teens or adults who are no longer growing. Epiphyseal stapling. An operation to slow the rate of growth of the longer limb by inserting staples into the growth plate, then removing them when the desired result is achieved. Epiphysiodesis. An operation to slow the rate of growth of the longer limb by creating a permanent bony ridge near the growth plate. Limb lengthening. A procedure (also called distraction osteogenesis or the Ilizarov procedure) that involves attaching an internal or external fixator to a limb and gradually pulling apart bone segments to grow new bone between them. There are several ways your doctor can predict the final LLD, and thus the timing of the surgery. The easiest way is the so-called Australian method, popularised by Dr. Malcolm Menelaus, an Australian orthopedic surgeon. According to this method, growth in girls is estimated to stop at age 14, and in boys at age 16 years. The femur grows at the rate of 10 mm. a year, and the upper tibia at the rate of 6 mm. a year. Using simple arithmetic, one can get a fairly good prediction of future growth. This of course, is an average, and the patient may be an average. To cut down the risk of this, the doctor usually measures leg length using special X-ray technique (called a Scanogram) on three occasions over at least one year duration to estimate growth per year. He may also do an X-ray of the left hand to estimate the bone age (which in some cases may differ from chronological age) by comparing it with an atlas of bone age. In most cases, however, the bone age and chronological age are quite close. Another method of predicting final LLD is by using Anderson and Green?s remaining growth charts. This is a very cumbersome method, but was till the 1970?s, the only method of predicting remaining growth. More recently, however, a much more convenient method of predicting LLD was discovered by Dr. Colin Moseley from Montreal. His technique of using straight line graphs to plot growth of leg lengths is now the most widely used method of predicting leg length discrepancy. Whatever method your doctor uses, over a period of one or two years, once he has a good idea of the final LLD, he can then formulate a plan to equalize leg lengths. Epiphyseodesis is usually done in the last 2 to 3 years of growth, giving a maximum correction of about 5 cm. Leg lengthening can be done at any age, and can give corrections of 5 to10 cm., or more.
Coping with Mortons Neuroma
Overview
 Morton's neuroma is a condition that affects one of the nerves that run between the long bones (metatarsals) in the foot. The exact cause is not certain. Symptoms include pain, burning, numbness and tingling between two of the toes of the foot. About a quarter of people just need simple treatments including modification of their footwear. Sometimes surgery is needed for long-standing (chronic) symptoms.
Morton's neuroma is a condition that affects one of the nerves that run between the long bones (metatarsals) in the foot. The exact cause is not certain. Symptoms include pain, burning, numbness and tingling between two of the toes of the foot. About a quarter of people just need simple treatments including modification of their footwear. Sometimes surgery is needed for long-standing (chronic) symptoms.
Causes
A Morton?s Neuroma are a result of complex biomechanical changes that occur in your feet. There are a number of theories as to the exact cause of the scarring and thickening, but it basically boils down to overload of the tissue structure. The body lays down scar tissue to try to protect the overloaded structure. Tight-fitting shoes may exacerbate a Morton?s Neuroma. Shoes such as high heels and shoes with tight toe boxes (eg womens fashion shoes and cowboy boots) are particularly damaging to the toes. These shoes have a sloping foot bed and a narrow toe box. The slope causes the front of the foot to bear your weight. The angle of the toe box then squeezes your toes together. Footwear is not the only cause of a Morton?s Neuroma. Injuries to the foot can also be a factor in developing the condition by changing your foot biomechanics. Poor foot arch control leading to flat feet or foot overpronation does make you biomechanically susceptible to a neuroma.
Symptoms
The most common presenting complaints include pain and dysesthesias in the forefoot and corresponding toes adjacent to the neuroma. Pain is described as sharp and burning, and it may be associated with cramping. Numbness often is observed in the toes adjacent to the neuroma and seems to occur along with episodes of pain. Pain typically is intermittent, as episodes often occur for minutes to hours at a time and have long intervals (ie, weeks to months) between a single or small group of multiple attacks. Some patients describe the sensation as "walking on a marble." Massage of the affected area offers significant relief. Narrow tight high-heeled shoes aggravate the symptoms. Night pain is reported but is rare.
Diagnosis
The physician will make the diagnosis of Morton's neuroma based upon the patient's symptoms as described above in an interview, or history, and a physical examination. The physical examination will reveal exceptional tenderness in the involved interspace when the nerve area is pressed on the bottom of the foot. As the interspace is palpated, and pressure is applied from the top to the bottom of the foot, a click can sometimes be felt which reproduces the patient's pain. This is known as a Mulder's sign. Because of inconsistent results, imaging studies such as MRI or ultrasound scanning are not useful diagnostic tools for Morton's neuroma. Thus the physician must rely exclusively on the patient's history and physical examination in order to make a diagnosis.
Non Surgical Treatment
The first step in treating Morton's Neuroma is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating and relieving the pain. The next step in treatment is to use an orthotic designed with a metatarsal pad. This pad is located behind the ball-of-the-foot to unload pressure, and relieve the pain caused by the neuroma.
If problem persists, consult your foot doctor.
Surgical Treatment
About one person in four will not require any surgery for Morton's neuroma and their symptoms can be controlled with footwear modification and steroid/local anaesthetic injections. Of those who choose to have surgery, about three out of four will have good results with relief of their symptoms. Recurrent or persisting (chronic) symptoms can occur after surgery. Sometimes, decompression of the nerve may have been incomplete or the nerve may just remain 'irritable'. In those who have had cutting out (resection) of the nerve (neurectomy), a recurrent or 'stump' neuroma may develop in any nerve tissue that was left behind. This can sometimes be more painful than the original condition.
Prevention
Women, particularly those who wear tight shoes, are at greatest risk for Morton?s neuroma. The best way to prevent the condition is to wear shoes with wide toe boxes. Tight, pointed shoes squeeze bones, ligaments, muscles and nerves. High heels may worsen the problem by shifting your weight forward. Over time, this combination can cause the nerves to swell and become painful.
 Morton's neuroma is a condition that affects one of the nerves that run between the long bones (metatarsals) in the foot. The exact cause is not certain. Symptoms include pain, burning, numbness and tingling between two of the toes of the foot. About a quarter of people just need simple treatments including modification of their footwear. Sometimes surgery is needed for long-standing (chronic) symptoms.
Morton's neuroma is a condition that affects one of the nerves that run between the long bones (metatarsals) in the foot. The exact cause is not certain. Symptoms include pain, burning, numbness and tingling between two of the toes of the foot. About a quarter of people just need simple treatments including modification of their footwear. Sometimes surgery is needed for long-standing (chronic) symptoms.Causes
A Morton?s Neuroma are a result of complex biomechanical changes that occur in your feet. There are a number of theories as to the exact cause of the scarring and thickening, but it basically boils down to overload of the tissue structure. The body lays down scar tissue to try to protect the overloaded structure. Tight-fitting shoes may exacerbate a Morton?s Neuroma. Shoes such as high heels and shoes with tight toe boxes (eg womens fashion shoes and cowboy boots) are particularly damaging to the toes. These shoes have a sloping foot bed and a narrow toe box. The slope causes the front of the foot to bear your weight. The angle of the toe box then squeezes your toes together. Footwear is not the only cause of a Morton?s Neuroma. Injuries to the foot can also be a factor in developing the condition by changing your foot biomechanics. Poor foot arch control leading to flat feet or foot overpronation does make you biomechanically susceptible to a neuroma.
Symptoms
The most common presenting complaints include pain and dysesthesias in the forefoot and corresponding toes adjacent to the neuroma. Pain is described as sharp and burning, and it may be associated with cramping. Numbness often is observed in the toes adjacent to the neuroma and seems to occur along with episodes of pain. Pain typically is intermittent, as episodes often occur for minutes to hours at a time and have long intervals (ie, weeks to months) between a single or small group of multiple attacks. Some patients describe the sensation as "walking on a marble." Massage of the affected area offers significant relief. Narrow tight high-heeled shoes aggravate the symptoms. Night pain is reported but is rare.
Diagnosis
The physician will make the diagnosis of Morton's neuroma based upon the patient's symptoms as described above in an interview, or history, and a physical examination. The physical examination will reveal exceptional tenderness in the involved interspace when the nerve area is pressed on the bottom of the foot. As the interspace is palpated, and pressure is applied from the top to the bottom of the foot, a click can sometimes be felt which reproduces the patient's pain. This is known as a Mulder's sign. Because of inconsistent results, imaging studies such as MRI or ultrasound scanning are not useful diagnostic tools for Morton's neuroma. Thus the physician must rely exclusively on the patient's history and physical examination in order to make a diagnosis.
Non Surgical Treatment
The first step in treating Morton's Neuroma is to select proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating and relieving the pain. The next step in treatment is to use an orthotic designed with a metatarsal pad. This pad is located behind the ball-of-the-foot to unload pressure, and relieve the pain caused by the neuroma.
If problem persists, consult your foot doctor.

Surgical Treatment
About one person in four will not require any surgery for Morton's neuroma and their symptoms can be controlled with footwear modification and steroid/local anaesthetic injections. Of those who choose to have surgery, about three out of four will have good results with relief of their symptoms. Recurrent or persisting (chronic) symptoms can occur after surgery. Sometimes, decompression of the nerve may have been incomplete or the nerve may just remain 'irritable'. In those who have had cutting out (resection) of the nerve (neurectomy), a recurrent or 'stump' neuroma may develop in any nerve tissue that was left behind. This can sometimes be more painful than the original condition.
Prevention
Women, particularly those who wear tight shoes, are at greatest risk for Morton?s neuroma. The best way to prevent the condition is to wear shoes with wide toe boxes. Tight, pointed shoes squeeze bones, ligaments, muscles and nerves. High heels may worsen the problem by shifting your weight forward. Over time, this combination can cause the nerves to swell and become painful.
Chiropodists Prefer Shoe Lifts For Leg Length Difference
There are actually two different kinds of leg length discrepancies, congenital and acquired. Congenital implies that you are born with it. One leg is anatomically shorter in comparison to the other. Through developmental phases of aging, the human brain picks up on the step pattern and recognizes some variation. Our bodies typically adapts by dipping one shoulder over to the "short" side. A difference of under a quarter inch isn't grossly uncommon, doesn't need Shoe Lifts to compensate and generally does not have a profound effect over a lifetime.

Leg length inequality goes mainly undiscovered on a daily basis, however this problem is simply remedied, and can reduce a number of cases of back pain.
Treatment for leg length inequality usually consists of Shoe Lifts. These are cost-effective, often priced at below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most prevalent condition affecting men and women today. Over 80 million men and women experience back pain at some stage in their life. It's a problem that costs companies huge amounts of money every year due to lost time and productivity. New and more effective treatment solutions are continually sought after in the hope of reducing the economical impact this issue causes.

People from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these types of cases Shoe Lifts can be of very useful. The lifts are capable of easing any pain and discomfort in the feet. Shoe Lifts are recommended by many specialist orthopaedic orthopedists.
So as to support the body in a well balanced manner, your feet have got a vital part to play. In spite of that, it's often the most overlooked zone of the body. Some people have flat-feet meaning there is unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be impacted too. Shoe Lifts make sure that ideal posture and balance are restored.

Leg length inequality goes mainly undiscovered on a daily basis, however this problem is simply remedied, and can reduce a number of cases of back pain.
Treatment for leg length inequality usually consists of Shoe Lifts. These are cost-effective, often priced at below twenty dollars, in comparison to a custom orthotic of $200 or even more. When the amount of leg length inequality begins to exceed half an inch, a whole sole lift is generally the better choice than a heel lift. This prevents the foot from being unnecessarily stressed in an abnormal position.
Upper back pain is easily the most prevalent condition affecting men and women today. Over 80 million men and women experience back pain at some stage in their life. It's a problem that costs companies huge amounts of money every year due to lost time and productivity. New and more effective treatment solutions are continually sought after in the hope of reducing the economical impact this issue causes.

People from all corners of the earth suffer the pain of foot ache due to leg length discrepancy. In these types of cases Shoe Lifts can be of very useful. The lifts are capable of easing any pain and discomfort in the feet. Shoe Lifts are recommended by many specialist orthopaedic orthopedists.
So as to support the body in a well balanced manner, your feet have got a vital part to play. In spite of that, it's often the most overlooked zone of the body. Some people have flat-feet meaning there is unequal force exerted on the feet. This causes other areas of the body including knees, ankles and backs to be impacted too. Shoe Lifts make sure that ideal posture and balance are restored.
Help For Contracted Toes Feet
 Overview
Overview
Essentially, there's one consistent type of Hammer toe, the condition in which your toes are contracted into a hammer or upside-down "V" shape. However, depending on its severity, hammertoe is characterized into two forms. Flexible hammertoe is hammertoe in which the joints of the toes are still moveable or flexible and can be treated with nonsurgical therapies. Rigid hammertoe is the more serious condition in which the joints' muscles and tendons have lost any flexibility and the contraction cannot be corrected by nonsurgical means. As a result, surgery is generally required to deal with the problem. This is why it's important to consult a physician as soon as the problem is recognized for the possibility of successful nonsurgical treatment.
Causes
A person may be born with hammer toe or may develop it from wearing short, narrow shoes. Hammer toe can occur in children who outgrow shoes rapidly. Sometimes hammertoes hammer toe is genetic and is caused by a nerve disorder in the foot. High heeled shoes are can also cause hammer toe. The reason for this is that the toes are not only bunched up, but the weight of the body is pushing them forward even further.
 Symptoms
Symptoms
Symptoms may include pain in the affected toe or toes when you wear shoes, making it hard or painful to walk. A corn or callus on the top of the joint caused by rubbing against the shoe. Swelling and redness of the skin over the joint. Trouble finding comfortable shoes.
Diagnosis
A hammertoe is usually diagnosed with a physical inspection of your toe. Imaging tests, such as X-rays, may be ordered if you have had a bone, muscle, or ligament injury in your toe.
Non Surgical Treatment
Symptomatic treatment of hammertoes consists of such things as open toed shoes or hammertoe pads. There are over the counter corn removers for temporally reducing the painful callous often seen with the hammertoe. These medications must be used with caution. They are a mild acid that burns the callous off. These medications should never be used for corns or callouses between the toes. Persons with diabetes or bad circulation should never use these products.
Surgical Treatment
There are several surgical techniques used to treat hammertoes. When the problem is less severe, the doctor will remove a small piece of bone at the involved joint and realign the toe joint. More severe hammer toes may need more complicated surgery.